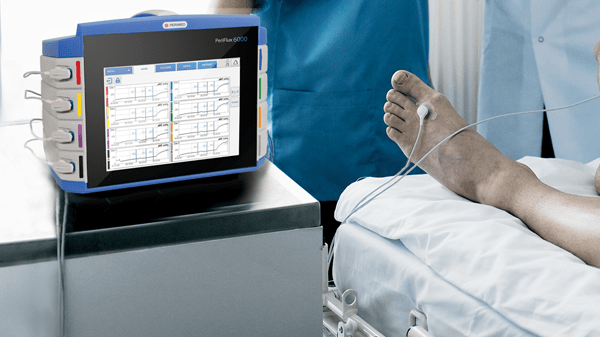
TCM5 FLEX transcutaneous monitor
Transcutaneous monitor for monitoring oxygenation and ventilation in critically ill patients
-
 Automatic temperature regulation
Automatic temperature regulation
-
 Real-time information
Real-time information
-
 Visible alerts
Visible alerts
TCM5 FLEX transcutaneous monitor supports your care of critically ill patients
The TCM5 FLEX transcutaneous monitor is a compact, easy-to-use solution that delivers accurate and continuous measurement of oxygenation (tcpO2) and ventilation (tcpCO2) status in neonatal, pediatric and adult patients in the ICU.
System defined limits of site time vs. temperature help reduce the risk of harm from the heated electrode.


Parameters
Oxygen saturation, reported as a percentage of oxyhemoglobin (HbO2) on a total of oxy- and deoxy-hemoglobin. It is expressed by the formula: HbO2 / (HbO2+deoxyhemoglobin). It is measured non-invasively by pulse oximetry, an absorption-based technique. The relationship between SpO2 (measured by pulse oximetry) and pO2 is given by the oxygen dissociation curve.
tcpCO2 is measured through a sensor placed on the skin surface. A tcpCO2 sensor uses the Stow-Severinghaus principle. CO2 reacts with water and forms carbonic acid and dissociates into H+, which is interpreted through a pH glass element. After conversion, the sensor algorithm generates a tcpCO2 in mmHg (millimeters of mercury) or kPa (kilopascals)
tcpO2 is measured through a sensor placed on the skin surface.
A tcpO2 sensor is based on the Clark principle; O2 diffuses through the skin and the membrane to a Platinum cathode. After conversion, the sensor algorithm generates a tcpO2 in mmHg (millimeters of mercury) or kPa (kilopascals).


A transcutaneous monitor that helps you focus on patient care
The TCM5 FLEX transcutaneous monitor has an intuitive user interface and built-in tutorials that make it easy to set up, learn and use.
Compact and practical, the TCM5 FLEX monitor comes with a color touchscreen. Clear on-screen messages give you an immediate overview of measured parameters supporting patient care.
A clearly visible alarm bar on top of the monitor and on-screen icons alert you to changes in patient status. Real-time trending measurements allow for immediate clinical intervention to critical changes in patient status. [1]
Click here to renew consent
Connect your TCM5 device and see patient data on one screen
![]()
Connectivity options


Transcutaneous monitor with reliable sensors
The surgical steel protected sensors measure tcpO2 and tcpCO2, SpO2 and pulse rate, delivering consistent and reliable results. The sensors have a variety of fixation options helping to improve patient comfort.
Automatic calibration of the sensor reduces preparation time and improves workflow.
A dedicated sensor cable spool makes cable management easy, keeping your department clutter-free.
New for 2022: Improved sensor head design with better protection of the cable and greater pull strength.


Transcutaneous monitoring enables careful monitoring of the neonate
Transcutaneous monitoring – or continuous, non-invasive monitoring – of tcpO2 and tcpCO2 can detect changes in the oxygenation and ventilation status of neonates. [2, 3, 4, 5]
Transcutaneous monitoring complements arterial and capillary blood sampling. You can reduce the number of blood samples and limit unnecessary handling of the infant, while ensuring careful control of your patient. [3, 4, 5, 6, 7]
The TCM5 FLEX transcutaneous monitor helps reduce patient discomfort with system defined limits of site time vs. temperature to reduce the risk of harm from the heated electrode by predefined combinations of time and temperature.
Continuous transcutaneous monitoring of patients in the ICU
Patients with acute respiratory failure and respiratory pump insufficiency are often treated with mechanical ventilation. Real-time monitoring offers a reliable approach to titrate ventilator settings without repeated blood sampling.[8, 9, 10, 11]
Unlike blood gas sampling, transcutaneous monitoring provides continuous information on CO2 levels allowing for proactive, rather than reactive ventilator adjustments.[10]
Transcutaneous monitoring improves patient care by reducing the need for blood samples, thereby reducing patient discomfort.[7, 10]
Weaning and extubation decisions may be made based on tcpCO2 measurement alone.[10]




By being able to view continuous data instead of having to rely on periodic blood gas analysis, I feel fully confident in my ability to be precise and accurate so I can provide a higher level of care.
- Dr. Marco Bardessono, Pulmonologist at the A.O.U. Citta della Salute e della Scienza hospital in Torino, Italy
Related products and solutions
Related knowledge sources
Related on-demand webinars
Combining blood gas invasive and non-invasive monitoring for the best care of our neonates
Presented by Dr. Kaare E. Lundstrøm
TC monitoring in NICU - the value of tcpO2
Presented by Daniele De Luca (MD,PhD)
References
1. Spelten O. Transcutaneous PTCCO2 measurement in combination with arterial blood gas analysis provides superior accuracy and reliability in ICU patients. J Clin Monit Comput (2017) 31:153–158.
2. Quine D, Stenson BJ. Does the monitoring method influence stability of oxygenation in preterm infants? A randomised crossover study of saturation versus transcutaneous monitoring. Arch Dis Child Fetal Neonatal 2008; 93.
3. Rüdiger M et al. A survey of transcutaneous blood gas monitoring among European neonatal intensive care units. BMC pediatrics 2005; 5, 30.
4. Sandberg KL et al. Transcutaneous blood gas monitoring during neonatal intensive care. Acta pæediatrica 2011; 100.
5. SØRENSEN L, BRAGE-ANDERSEN L, GREISEN G. Effects of the transcutaneous electrode temperature on the accuracy of transcutaneous carbon dioxide tension. Scandinavian Journal of Clinical and Laboratory Investigation 2011; 71, 7: 548-52.
6. Goenka A et al. Neonatal blood gas sampling methods. SAJCH 2012; 6, 1.
7. Lundstrøm K. E. Continous Blood gas monitoring in neonates and infants. neonatal INTENSIVE CARE 2003; 16, 4.
8. Jardins TD, Burton GB. Clinical manifestations and assessment of respiratory disease. 6th edition. Maryland Heights: MOSBY Elsevier, 2011; 125.
9. Windisch W et al. German National Guideline for Treating Chronic Respiratory Failure with Invasive and Non-Invasive Ventilation: Revised Edition 2017 – Part 1. Respiration 2018; 1-32.
10. Restrepo RD. AARC Clinical Practice Guideline: Transcutaneous Monitoring of Carbon Dioxide and Oxygen. Respiratory Care, 2012; 57, 11: 1956.
11. Jansenss JP. Transcutaneous PcO2 to Monitor Noninvasive Mechanical Ventilation in Adults. Chest 1998; 113: 768-73.
Cookies are used on this website
Use of cookiesPlease enter a valid email
We will be sending an e-mail invitation to you shortly to sign in using Microsoft Azure AD.
It seems that your e-mail is not registered with us
Please click "Get started" in the e-mail to complete the registration process
Radiometer is using Microsoft AZURE Active Directory to authenticate users
Radiometer uses Azure AD to provide our customers and partners secure access to documents, resources, and other services on our customer portal.
If your organization is already using Azure AD you can use the same credentials to access Radiometer's customer portal.
Key benefits
- Allow the use of existing Active Directory credentials
- Single-sign on experience
- Use same credentials to access future services
Request access
You will receive an invitation to access our services via e-mail when your request has been approved.
When you accept the invitation, and your organization is already using AZURE AD, you can use the same credentials to access Radiometer's customer portal. Otherwise, a one-time password will be sent via e-mail to sign in.